Abstract
Introduction: Addition of tyrosine Kinase inhibitors (TKI) to induction chemotherapy in management of Philadelphia chromosome positive (Ph+) ALL has significantly improved remission rates prior to allogeneic HSCT compared to the pre-TKI era. Consolidation with HSCT further prolongs remission and is potentially curative in the majority of patients. However, relapse is the commonest cause of treatment failure post HSCT with the highest incidence occurring within 18 months post-transplant. One possible strategy to minimize the risk of relapse is to commence TKI maintenance early post transplantation; which is increasingly becoming a common practice in many centers. However long term efficacy of this approach has not been established.
Methods: A retrospective search for Ph+ ALL patients undergoing allogeneic HSCT from March 2001 to September 2015 (n=150) at our center was performed. From this cohort to determine the impact of prophylaxis we identified a subgroup of patients (n=99) who were in complete molecular response (CMR) before day +90 post HSCT. Subsequently we performed a day +90 landmark analysis to examine the outcome for patients according to whether or not they had commenced TKI maintenance by day +90 in a univariate and multivariate model. TKI maintenance was recommended but the final decision was based on feasibility and patient/physician preference.
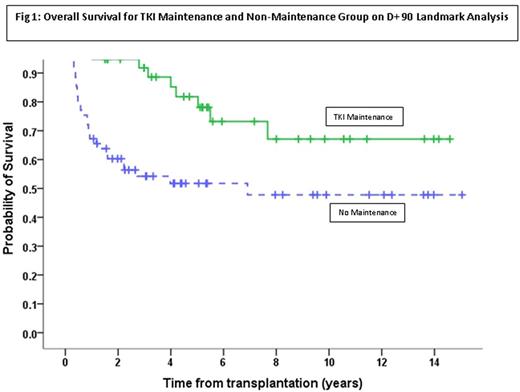
Results: Of the 99 patients included in the landmark analysis, 58.6% were men and 41.4% were women. Median age of study participants at the time of HSCT was 40 (range 3-64) years with a median follow up duration of 5.2 (range 1.1-15.0 ) years. At time of HSCT, 74.7% patients were in CR1, 16.2% were in CR2, and 9.1% were beyond CR2 or had primary induction failure. The majority of patients (97%) received a myeloablative preparative regimen, including radiation therapy in 31.3%. The median duration of TKI maintenance was 12.1 months (range 1-74 months). Imatinib was the commonest TKI used. Patients who received TKI maintenance (n=38) had superior 10-year probability of PFS and OS compared to patients who did not receive maintenance (n=61) at 68.1% vs 44.8%, p=0.005, and 67.1% vs 47.8%, p=0.004, respectively (Figure 1). TKI maintenance (HR=0.282, CI=0.122-0.654, p=0.001) and disease status pre-HSCT (beyond CR1) (HR=2.909, CI=1.286-6.577, p=0.01) were the two independent predictors for PFS in the multivariate model. Similarly, TKI maintenance (HR=0.244, CI=0.098-0.608, p=0.001) and disease status pre-HSCT (beyond CR1) (HR=3.394, CI=1.449-7.948, p=0.03) were the two independent predictor for OS. Both groups appeared to be well matched for several transplant/disease/treatment related variables.
Conclusion: Prophylactic TKI maintenance early post allo-SCT is feasible and is associated with improved PFS and OS. Future prospective studies are needed to define the optimal duration of TKI maintenance to further improve outcomes for this historically adverse group.
Oran: Celgene: Research Funding; AROG: Research Funding; Astex: Research Funding. Jabbour: Bristol-Myers Squibb: Consultancy. Kantarjian: Bristol-Meyers Squibb: Research Funding; Pfizer: Research Funding; Novartis: Research Funding; Amgen: Research Funding; ARIAD: Research Funding; Delta-Fly Pharma: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal